Just last week, HHS OIG issued a Fraud Alert warning that “Physicians who enter into compensation arrangements such as medical directorships must ensure that those arrangements reflect fair market value for bona fide services the physicians actually provide.” Then yesterday, the Department of Justice (DOJ) and HHS OIG announced a record setting $17 million False Claims Act settlement of a whistleblower case against Hebrew Homes Health Network, Inc. alleging that the company improperly paid doctors ostensibly acting as medical directors for referrals of Medicare patients requiring skilled nursing care.
Medical Directorships Can Be A Cover For Illegal Referrals
Bona fide Medical Directors perform a valuable function at a hospital or a nursing facility. However, the position can also be a cover for doctors to steer their patients to a particular facility. For example, in the Hebrew Homes case:
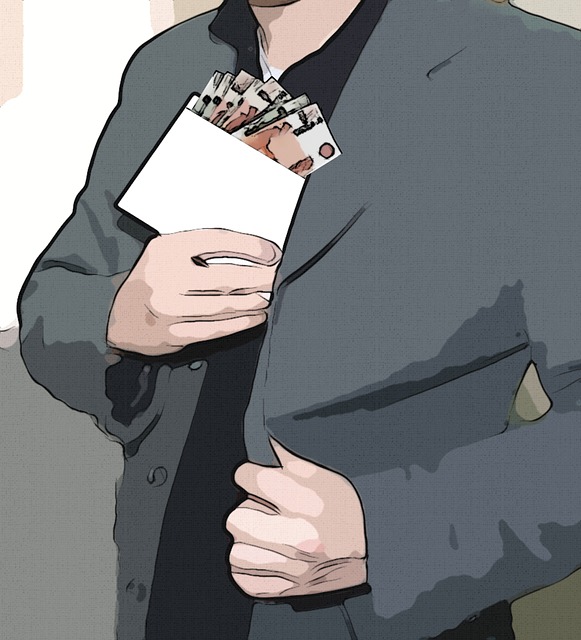
From 2006 through 2013, Hebrew Homes allegedly operated a sophisticated kickback scheme in which they hired numerous physicians ostensibly as medical directors pursuant to contracts that specified numerous job duties and hourly requirements. The various facilities had several such medical directors under contract at any given time, paying each several thousand dollars monthly. The United States alleged that in reality these were ghost positions, and that most of the medical directors were required to perform few, if any, of their contracted job duties. Instead, they were allegedly paid for their patient referrals to the Hebrew Homes facilities, which increased exponentially once the medical directors were put on the payroll.
Medical Directorships Can Violate The Anti-Kickback Statute and Stark Law
We have written before about the importance of Anti-Kickback Statute and its close cousin the Stark Act, and this recent settlement is a perfect example of the evils each law seeks to prevent or punish. In a nutshell, the Anti-Kickback Statute (42 U.S.C. § 1320a-7b(b)) prohibits the making or offering or paying or accepting “remuneration” (defined as any thing of value) if one purpose of the payment is to induce referrals. Stark (42 U.S.C.§1395nn), on the other hand, prohibits a hospital (or other entity providing health care items or services) from submitting claims to Medicare or Medicaid for items or services rendered to patients referred by physicians who have improper financial relationships with the providers of the items or services.
Each law contains certain “safe harbors” which are in essence exceptions to their blanket prohibitions. A violation of each law can be the basis for a civil (e.g., under the False Claims Act) prosecution by DOJ, civil penalties, or an administrative action by HHS. In addition, the Anti-Kickback Act provides criminal penalties. Congress designed both laws to ensure that physicians’ judgment about their patients’ care is conflict free. For example, as to whether an item or service is medically necessary, safe, effective, and of good quality. Congress wanted to keep the competitive playing field for health care providers level and fair, and to protect the financial integrity of government health care programs such as Medicare and Medicaid.
Illegal Referral Arrangements Violate the False Claims Act
We expect this most recent settlement, coupled with HHS OIG’s recent Fraud Alert, signals an increase in whistleblower cases and investigative and enforcement actions against hospitals, skilled nursing facilities, and other medical facilities that utilize physicians as medical directors. However, we are not certain if the government will also focus on the physicians.
As the saying goes, “It takes two to tango” and without physicians willing to accept kickbacks and break self-referral laws, the facilities could not play the game. In the most recent announced settlement, only the facility (Hebrew Homes) is paying to settle. While HHS OIG’s Fraud Alert notes that it has recently reached settlements with 12 individual physicians, these were administrative settlements under the Civil Monetary Penalties Law, not False Claims Act or criminal charges. We will see whether the individual physicians face False Claims Act liability for the improper medical directorships.